invasive investigation. However, it has to be clinically relevant. Example: Start with a physical exam, follow with basic lab tests like TSH and FT4, and proceed to imaging or more advanced diagnostics based on the results.
requires nuance.
Example: Initiate treatment immediately in severe cases rather than waiting for confirmatory tests, if clinical judgment strongly supports a particular diagnosis. For example, if a patient presents to ER with anaphylaxis, give epinephrine immediately instead of waiting for allergy tests or other investigations.
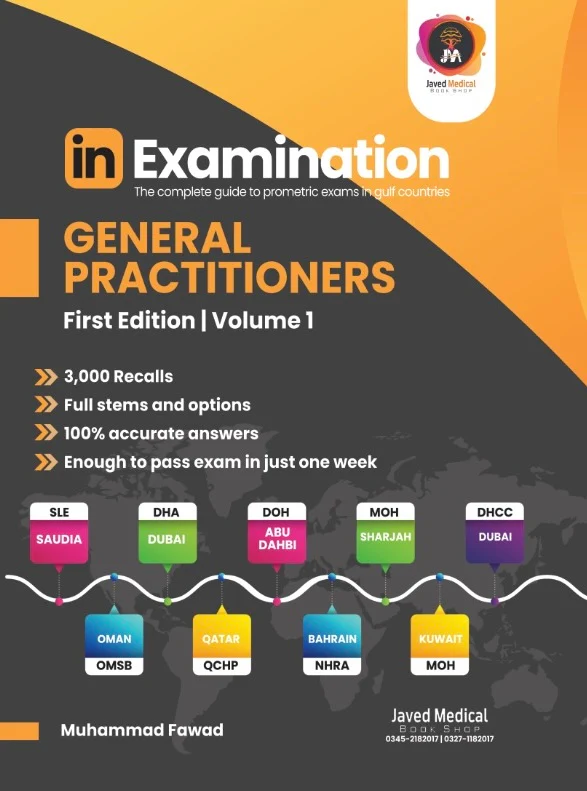
A lot of questions in the Qbank are bad recalls, so keep this in mind as you study.
Thyroid
First, we have to do a physical exam for assessment, followed by TSH and FT4, then it depends on the TSH value.
Low TSH
Do a thyroid scan to check the uptake in a hyperthyroidism case No uptake -> Subacute thyroiditis (has neck pain)
Diffuse -> Graves (also if positive antibody) Nodular if single, multinodular goiter if multiple nodules.
Always initiate treatment for hot nodules with an antithyroid drug first to reach euthyroid status (prevent thyroid storm), followed by RAI or surgery. Go with near total thyroidectomy if compressive symptoms exist (such as dysphagia), or if the patient failed medical treatment, or if they have exopthalmos. Medically, if you had to choose between beta blockers and an antithyroid drug, go with beta blockers first for symptomatic treatment. Pregnant in the first trimester?
Choose propylthiouracil.
Only choose FNA for cold solid nodules.
Normal or high TSH
Ultrasound to assess the nodule/s, then FNA nodules if the size is 1*1cm or bigger. If both nodules are smaller than that, follow up with ultrasound.
Afterwards, it depends on the Bethesda classification for cold thyroid nodules:
If a diagnosis of hypothyroidism is made, start levothyroxine and reassess after 6 weeks. Titrate the dose depending on the follow up visit.
If the TSH isn’t mentioned in the question, pretend that it’s normal. Always follow the approach step by step. If the TSH is normal and there’s clinical suspicion, repeat TSH unless there’s a history of radiofrequency ablation.
Thyroid cancer follow up
Most common thyroid cancer associated with autoimmune thyroiditis is Lymphoma (not Lymphoblastic) followed by Papillary.
Neck nodule
Thyroglossal cyst (central) moves with tongue protrusion.
Treated surgically.
Cystic hygroma (lateral) has clear lymphatic fluid. The initial treatment is sclerotherapy, best is surgical.
Low TSH case. In other words it’s hyperthyroidism thus the next step is thyroid scan.
A- antithyroid drug
B- RT thyroidectomy
C- Hemithyroidectomy
D- radioactive iodine
Achieve euthyroid status first with an antithyroid medication, then go for radioactive iodine, or near total thyroidectomy if there is presence of eye symptoms or compressive symptoms.
(right sides 1/2cm), which of the following is the best management?
A- Right hemithyroidectomy.
B- Subtotal thyroidectomy.
C- Near-total thyroidectomy.
D- Radioactive ablation.
Near total thyroidectomy due to the presence of eye symptoms. Can’t find near-total in the options? Go with total.
As explained earlier, we only take samples from solid nodules. In another recall, let’s say you had to choose between FNA cystic and biopsy solid, go for biopsy solid.
The sizes are in CM, and they’re both bigger than 1*1cm, so we need to FNA both.
Because both are smaller than 1*1cm.
Side note: lobectomy = hemithyroidectomy.
1.5*2 cm cold mass, FNA cytology revealed suspicious follicular neoplasm, which of the following the best initial management?
Follicular neoplasm = Bethesda 4, so go for hemithyroidectomy.
As explained earlier, never proceed with surgery until you achieve euthyroid status.
A- Papillary.
B- Medullary.
C- Anaplastic.
D- Lymphoma.
Lymphoma. If not present, go with papillary. If you see lymphoblastic in the options, then it’s wrong.
Calcitonin? Medullary thyroid cancer.
A- serial post op US
B- calcitonin
C- TSH , T3 , T4
D- Thyroglobulin
Papillary and follicular are followed up by thyroglobulin. But if it was medullary cancer? Go with calcitonin.
This is a case of papillary thyroid cancer metastasizing to the lymph nodes.
A- Completion thyroidectomy.
B- Follow up 3 months.
C- RAI.
D- Lobectomy.
Since the size is only 8mm, simply follow up. We go with total thyroidectomy if it’s 1cm or bigger.
A- Cricothyrotomy
B- Re-intubate.
C- Nasal canula.
D- Bedside tracheostomy.
A case of bilateral vocal cord paralysis post-thyroidectomy. Requires immediate reintubation.
A- Take her back to OR.
B- Bedside tracheostomy.
C- Nasal cannula.
D- Bedside wound exploration.
This question has a few different recalls when it comes to the wording in the answers. The correct answer is opening the wound immediately due to the hematoma.
High pitched voice = superior laryngeal nerve.
Hoarseness = recurrent laryngeal nerve.
What is the appropriate management?
A- Surgery
B- Observation
C- Chemotherapy
D- Radiotherapy
This is a case of cystic hygroma, a lateral neck mass with clear lymphatic fluid. Initial: sclerotherapy. Best: surgery
Midline mass and moves with tongue protrusion. Another recall asking about management? Go with surgery.
A- thyroidectomy.
B- radioactive iodine.
C- propranolol.
D- methimazole.
What’s the diagnosis?
A-Graves disease
B-Sick euthyroid sickness C-Hashimoto thyroiditis
D-Subacute thyroiditis
Because of the lab values.
the doctor raised the dose to 200 mcg. She is otherwise normal (see labs). Labs: T4 (normal) T3 (normal)
TSH= 17 (high). What is the best explanation for the lab findings?
Normal T4 + High TSH = Poor compliance. T4 improves quickly by taking levothyroxine, but the TSH requires daily compliance long term or it will continue to stay high. If the patient had actual good compliance and the TSH is still high? Then we need to increase the dose 6 weeks after the last appointment.
In real life, you would start both methimazole and propanolol at the same time. In the exam, though go for propanolol first for symptomatic relief.
A- Sub total thyroidectomy
B- Total thyroidectomy
C- Hemithyroidectomy
Follow the Bethesda classification. Case of thyroid cancer? Go for near total thyroidectomy. If that’s not available in the options, go for total thyroidectomy.
A thyroid goiter that led to compressive symptoms (dysphagia). The patient needs surgery.
A- Give analgesia.
B- Take blood pressure again.
C- Check calcium level.
D- Administer Calcium Gluconate.
Hypocalcemia as a complication of thyroidectomy.
a-Repeat FNA b-Scan
c-Remove thyroid
d-Follow up
Inadequate FNA means the Bethesda score is 1, so you have to repeat FNA now.
Breast
Triple assessment approach
The first step in evaluation is physical examination followed by imaging, then biopsy. Go with ultrasound for patients under 40 years old, and mammography for older patients. If the patient has a positive family history of a first degree relative 10 years older, choose mammography even if the patient is in their 30s.
Afterwards, go with core needle biopsy to confirm the diagnosis. In a breast case, only choose FNA for cystic lesions.
BI-RAD
0 – additional imaging required
1 and 2 – annual screening
3 – follow up imaging in 6 months
4 and 5 – core biopsy
6 – surgery
Mammography screening is done annually in the range of 40 to 50 years old. Afterwards, every two years according to the USPSTF.
A core needle biopsy showing intraductal hyperplasia? Go with WLE.
Fibroadenoma -> oval shape, mobile mass, related to the menstrual cycle. Treated with WLE.
Phyllode -> rapidly growing, not related to the menstrual cycle. Treated with WLE if benign phyllode, or simple mastectomy if malignant, or 8*8cm+
Choose CT with contrast first in a malignant case for staging.
Intraductal papilloma -> most common cause of non-lactating nipple discharge. Bloody.
Duct ectasia -> inverted nipple, green discharge. Both ectasia and papilloma are treated with intraductal excision.
Fibrocystic changes -> multiple bilateral small masses, milky discharge, painful.
Fat cyst/necrosis -> skin retraction overlying the breast in addition to ecchymosis.
Montgomery follicles -> non-tender lumps confined to the areola.
Paget disease -> rare cancer. Unilateral involvement: 1) Erythematous 2) Pruritis 3) Nipple destruction. Treated by mastectomy with SLNB.
Ductal Carcinoma In Situ (DCIS) -> mastectomy with SLNB, or WLE with radiation.
Lobular Carcinoma In Situ (LCIS) -> interval screening/close surveillance.
Family history
BRCA is an autosomal dominant gene mutation associated with an increased risk for early onset breast and ovarian cancer. If suspected in first degree relatives, first screen the affected patients with cancer to confirm, then screen the entire family.
BRCA positive screening
Skin tethering is a keyword for a patient with breast cancer.
Atypia is the most significant risk factor.
Inflammation
An erythematous firm swelling is mastitis. It’s treated with antibiotics.
However, if the patient has a fluctuant mass, of if there’s any skin changes besides redness, then it’s an abscess.
Abscess
If one of the following is present then choose I+D Multiple, 5cm or more, thinned, ischemic or necrotic skin. Otherwise, aspiration is enough.
A- CT
B- MRI
C- US
D- Mammogram
Since the patient is younger than 40 years old, we go for an US.
was 43, asking about screening?
Because of family history, start mammography 10 years prior to her mother’s onset of breast cancer. No family history? Wait until she is 40 years old.
Triple assessment approach. Imaging was done, so the next step is biopsy.
In a typical breast case, after going for imaging the next step is biopsy. However, this patient has physiologic bilateral nipple discharge which could have a variety of different colors, but the most important keyword is multiple ducts and bilateral. If it was unilateral + green = a clear case of duct ectasia so only then we would choose biopsy.
Bloody nipple discharge indicates a case of intraductal papilloma.
A-duct excision
B-core needle biopsy C-galactography
D-mastectomy
Bad recall, but it’s certainly a case of intraductal papilloma (bloody) rather than duct ectasia (green). Although both are treated similarly, if we had a case of bilateral green discharge then that’s physiological. In the case of papilloma? It can be bilateral or unilateral.
A- mammogram annually
B- start ultrasound
C- MRI
Due to her age it should be mammography now, not annually. If it comes like this go with US. We only go with an MRI if both mammography and US are negative.
The report was as follows:US: can’t remember the details) Comment: BI-RADS III / propably benign
CT: multiple fibrous tissues with no calcifications How will you nanage this patien?
A-Follow up after 6 months
B-Core biopsy C-MRI breast
Core needle biopsy, also referred to as true-cut biopsy in some recalls. Be sure to review the BI-RAD scores.
What is the appropriate management ?
A- chemo
B- radio
C- mastectomy
D- MRM
As explained at the start of this section, we go for a simple mastectomy due to the size.
and showed malignant phyllode tumor, what’s the next appropriate step?
As this is a case of malignant phyllodes, we need to go for chest CT with contrast first to stage the cancer, but since the option here is without contrast go for simple mastectomy.
A- WLE
B–mastectomy
In a malignant case, we either go for WLE with radiation or mastectomy. It would be preferred to go for WLE with radiation due to the small size so we can conserve the cosmetic appearance of the breast, but it’s missing here.
B-1y C-2y D-3y
Mammography screening is done annually in the range of 40 to 50 years old. Afterwards, every two years according to the USPSTF.
The keyword is atypical ductal hyperplasia.
Both Fibroadenoma and Phyllodes continuously grow, but the difference is that Phyllodes grow rapidly and also cause thinning of the overlying skin.
A – breast cyst
B- fibroadenoma
C – fibrocystic cancer
D – intraductal carcinoma
An oval shaped mobile mass. A missing keyword is the relation between the mass and the menstrual cycle, unlike Phyllodes.
There’s another recall with multiple oval masses which is again, a case of fibroadenoma.
Another recall:
21 year old female presented to your clinic with a 2 month history of right breast lump. It started as 2 cm in size oval shaped and mobile lump. The lump size fluctuate around menstruation. What is the diagnosis?
The keyword is skin retraction overlying the breast in addition to ecchymosis.
Confined to the areola.
what is the next step?
imaging is core needle biopsy.
What would you recommend for her screening?
The patient is 35 years old, and her sister developed cancer at 45 years old, so start mammography 10 years early.
Since her sister developed breast cancer quite early, it makes us suspect BRCA. First, confirm that the affected patient has the gene, then start annually screening the entire family if the BRCA gene is positive.
A- FNA
B- core biopsy
C- exicional biopsy
D- reassess after
Another recall:
26 year old female presented with a tender breast lump. US was done and showed simple cyst. She does not have any family history for breast cancer. What is the best management?
We aspirate breast masses only in a case of cyst.
Fibroadenoma Duct ectasia
Carcinoma of breast
Breast cyst Skin tethering? This is cancer.
Her age
Presence of hyperplasia Presence of atypia Fibroadrnoma size
A— Radiotherapy B— Chemotherapy C— Mastectomy
D— High risk screening protocol
Both DCIS and invasive ductal are treated with surgery. However, if it were a case of LCIS, go with D.
A-flucloxacillin B-Aspiration C-I&D
Erythema, swelling, no other skin changes, and no fluctuation. Clear case of mastitis.
breast with swollen axillary lymph nodes. What is the most likely diagnosis?
A observation
B incision and drainage
C antibiotics
Due to the thinning of skin. In breast abscess, any skin changes aside from redness require I&D.
I had this question in my exam. In the full recall, the cyst was 3*4cm and there were no skin changes that warranted I&D.
Trauma
Chest trauma
Tension Pneumothorax
Hyperresonance on percussion and decreased breath sounds on the same side, tracheal shifting to the opposite side. Raised JVP. Treated by needle decompression.
Open Pneumothorax
Suspect it if you notice a suction sound from a lacerated wound, then go for three side dressing. If not in the options? Go for a chest tube.
Cardiac tamponade
Raised JVP, low BP (weak thread pulse), muffled heart sounds. Bilateral clear lungs. Treated by pericardiocentesis.
Hemothorax
Stony dull on percussion due to fluid, flat JVP (because of hypovolemia).
Treated by inserting a chest tube.
Flail chest
Multiple broken ribs and paradoxical breathing. No additional signs. Treated by analgesia + assisted ventilation.
Cardiac contusion
Signs of ecchymosis on the chest, bounding pulse, arrhythmia.
Pulmonary contusion
New lung infiltrates post MVA.
Tracheobronchial Injury
Similar to tension pneumothorax, but has signs of subcutaneous emphysema and pneumomediastinum. Diagnosed by a bronchoscopy.
Tube placement
Chest tube -> between the 4th and 5th ICS midaxillary line Therapeutic needle -> at the 2nd ICS midclavicular line
Diagnostic needle -> between the 8th and 10th ICS midaxillary line
Thoracotomy indication
1500ml after chest tube insertion, or 200-250cc within 2-4h
Abdominal trauma
STAB
Stable -> CT Unstable -> Laparotomy
BLUNT
Stable -> CT Unstable -> FAST
Approach to management after FAST as an initial step: Stable and positive -> CT
Stable and negative -> Routine examination
Unstable and positive -> Laparotomy Unstable and negative -> DPL
Immediate laparotomy:
Positive CT findings, Positive FAST if unstable, omentum is seen, evisceration, peritonitis, or abdominal rigidity.
Neck trauma
Zone 1 -> CT-A if +ve -> Endovascular repair
If +ve bronchogram or esophagram -> open repair Zone 2 and 3 if asymptomatic -> observe
Zone 2 symptomatic -> immediate open repair
Zone 3 symptomatic -> CT-A if +ve -> endovascular repair
Unstable (expanding hematoma, uncontrolled hemorrhage) = ligation in all zones
A-tension pneumothorax
B- hemothorax
C- cardiac temponade
Full recall. However, it’s enough to diagnose tension pneumothorax. Cardiac tamponade requires the beck’s triad: 1) low BP 2) muffled heart 3) raised JVP. As for hemothorax, suspect it if you find stony dullness on percussion and flat JVP. In our question, the JVP is distended. Tension pneumothorax is the most common presentation and all the details in the question lead us to it.
Clear case of tension pneumothorax.
Open pneumothorax. Initiate management with a three side dressing. Definitive treatment requires closure of the chest wall defect and a chest tube away from the site of injury.
Entry in both lungs. What’s the diagnosis?
The beck’s triad in this case is missing muffled heart sounds, but by exclusion tamponade is still the right answer. Equal bilateral lung sounds excludes pneumothorax which is unilateral. Weak thread pulse excludes cardiac contusion because it presents with a bounding pulse in addition to arrhythmia and ecchymosis. Side note: Weak thread pulse = low BP.
A-fluid bolus
B-Pericardiocentesis C-Immediate thoratom
The beck’s triad is present here.
 Patient sustained a chest stab wound injury, on examination there was Stony dullness over right chest and tracheal deviation to the left, what is the diagnosis?
Patient sustained a chest stab wound injury, on examination there was Stony dullness over right chest and tracheal deviation to the left, what is the diagnosis?Massive Hemothorax
Stony dull immediately excludes tension pneumothorax, as that one presents with hyperresonance. Hemothorax is treated with a chest tube.
Cardiac contusion
Strong bounding pulse, arrhythmia on ECG, and chest ecchymosis.
A- PE
B- flial chest
C- cardiac contusion D-
pulmonary contusions
The keyword is lung infiltrates.
Assisted ventilation
C. IV fluid.
Clear case of flail chest. A missing keyword which is most likely in the full recall is paradoxical breathing. Start management with analgesia, then go for assisted ventilation.
pneumomediastinum. What is the diagnosis
A- Tension pneumothorax
B- Open pneumothorax C-
Tracheobronchial injury
D- Hemopneumothorax
Subcutaneous emphysema and pneumomediastinum.
Fiberoptic bronchoscopy
Significant pneumomediastinum. Tracheobronchial injury is diagnosed by bronchoscopy.
widened mediastinum. What is the diagnosis?
Thoracic aorta rupture
D. Spontaneous pneumothorax
Mediastinal widening and expanded lungs in addition to tracheal shifting commonly present in a case of aortic injury. Side note: there’s another recall with ruptured esophagus instead of aortic rupture in addition to tracheal shifting to the left, but I believe it is a bad recall as the symptoms are not relevant.
Confirm placement of chest tube
Side note:
Chest tube -> between the 4th and 5th ICS midaxillary line Therapeutic needle -> at the 2nd ICS midclavicular line Diagnostic needle -> between the 8th and 10th ICS midaxillary line
1500ml or 200cc within 2-4 hours = thoracotomy.
A-Thoracentesis
B-Tube thoracostomy (chest tube) C-thoracotomy
BP: 90/67.
HR: 45 bpm.
What’s the next step?
urgent laparotomy.
A-
B- urgent thoracotomy.
Laparotomy is always done before thoracotomy. And now, we start with abdominal trauma below.
C- refer the patient to a hospital with vascular surgeon

 Patient presents with stab wound to the abdomen. After wound exploration, you found anterior abdominal fascia penetration. His vitals were stable. What is your next step?
Patient presents with stab wound to the abdomen. After wound exploration, you found anterior abdominal fascia penetration. His vitals were stable. What is your next step?A-
CT abdomen
B- MRI abdomen
C- Exploratory laparotomy
D- Diagnostic laparoscopy
Abdominal fascia penetration does not warrant laparotomy.
CT scan
Wound exploration is not correct. Go with CT and follow the ATLS.
All vitals normal except O2 90
What is the most appropriate management:
Thoracotomy
Tube thoracostomy
Expl lapratomy
Angioembolization
Positive FAST and the patient is stable, so the next step should be CT as we have no urgent need to rush to the OR just yet. By exclusion only, laparotomy.
CT report negative findings, Next step management:
Laparotomy
Omentum was seen, so go for laparotomy even if the patient is hemodynamically stable.
Ex lap
Unstable.

Since we already did FAST and the patient is stable go for CT scan. If the CT is positive go for laparotomy regardless of vital signs.
What is the next best step ?
DPL
D. FAST
Blunt trauma + unstable so we did FAST first, but since it’s negative we go for DPL this time.
Fast: positive for moderate fluid collection Bp: 90/50
He received 2L crystalloid without improvement What is next:
-Lavage
-Exploratory laparotomy
-Ct scan
Positive FAST and the patient is unstable.
C) CT scan abdomen D)
surgical exploration
Blunt + unstable so normally we would choose FAST. However, due to abdominal rigidity we need to go straight for laparotomy.

Restriction of spine movement
D. Pelvic binder
A similar recall: How to exclude cervical injury? Cervical CT scan.
Duodenal perforation
A)
Seatbelt + Chance fracture.
High spinal cord injury.
D. Tension pneumothorax. Low BP + low HR. Neurogenic shock.
A-Exploration B-US
C-X-RAY
D-CT Unclear question, but if the patient deteriorated it’s safe to assume laparotomy is a safe answer.
what is the best management?
Endovascular
C. Open and ligation
C. Angioembolization
 Appendicitis
Appendicitis
Appendicitis is the main cause of an acute surgical abdomen. The most common SMLE question is always about investigation. It depends on the age group, presentation length, and the Alvarado score.
Pediatric and female (reproductive age) -> US to avoid unnecessary radiation for children and a potentially pregnant woman. Order B-HCG to exclude pregnancy if it’s available in the choices, if not go with US.
Elderly (suspect cancer) and atypical lengthy presentation (suspect mass/ abscess/perforation) -> CT scan
In a typical male presentation, go with CT if the Alvarado score is 1-6. Go with laparoscopy if it’s 7-10.
Alvarado score
3 Symptoms -> Anorexia, N/V, shifting of pain to RLQ. 3 Signs -> RLQ tenderness, rebound tenderness, fever.
2 Labs -> Leukocytosis, left shift (neutrophils).
Each of them add a single point, except for RLQ tenderness and Leukocytosis, they add 2 points.
Signs
Rovsing’s = LLQ palpation causing RLQ pain Bluberg’s = rebound tenderness
Psoas = retro-cecal inflamed appendix Obturator = pelvic inflamed appendix
How to find the appendix during the surgery? Follow the taeniae coli.
If you go for an appendectomy and during the procedure you discover a normal appendix go ahead and search for Meckel’s diverticulum. Afterwards, what we do next depends:
If open -> proceed with appendectomy If lap -> leave the appendix
if you find an inflammation in the terminal ileum -> refer the patient to gastroenterology as it’s a case of IBD.
 Appendiceal mass
Appendiceal mass
Percutaneous drainage of the large collection then schedule for an interval appendectomy in 6 weeks.
Go for colonoscopy in an old age patient.
Appendiceal cancer
In adenocarcinoma, always go for a right hemicolectomy.
In carcinoid it depends:
1cm / tip of the appendix / no mesothelium invasion / no lymph node involvement -> Observe
2cm / base of the appendix / mesothelium invasion / lymph node involvement -> Right hemicolectomy
A- Appendicitis.
B- intussusception.
C- cholecystitis.
D- pancreatitis.
CT US
US is enough. No need to cause unnecessary radiation.
It could be ectopic, so with these choices go for an US next as it may be enough. Ideally, we would order a pregnancy test first then go for CT if the Alvarado score is less than 7 and the ectopic pregnancy has been excluded.
WBC high 14k
On US : inconclusive What is the next step ?
A- CT
B- open appendectomy
C- diagnostic laparoscopy
D- Transvaginal US
In this question, they already did an US and it was useless. Again, the correct answer should be pregnancy test. It seems to be a typical case of appendicitis but why rush to CT and cause potential harm if the patient turned out to be pregnant? Between these two options, the most likely answer is transvaginal US since not only is it the preferred way to diagnose an ectopic pregnancy, but it would also diagnose ovarian cysts. Lastly, the question specified “what is the next step” so in my opinion we should start with it first to rule out obgyn causes.
US has a limited role in obese patients. Open surgery makes no sense. Between B and D, I would go with CT scan as the “most appropriate management” once we order a pregnancy test first since the Alvarado score in this case is 6. As explained previously, the most appropriate management is not the same as the “most appropriate next step” so the answer here is CT scan.
A- laparoscopy
B- US
C- CT scan
In the full recall, this patient had an Alvarado score of 7, so we should go for laparoscopy. If less than that the answer changes to CT.
football. His WBC count 6 (normal), INR 1.1 (normal). Which of the following is the most appropriate next investigation?
A – CT abdomen
B – No need for further investigation, and follow up after 1 week
C – US or Xray
Most common cause
They did not specify the location, but the most common cause is appendicitis.
A- Gastritis
B- Pancreatitis
C- Cholecystitis
D- Appendicitis
Here, they specified RUQ which often means a case of cholecystitis. However, keep in mind that the appendix changes its location upwards in the third trimester. According to the recall, our patient is in the second trimester but it could be a bad recall and the patient is actually in the 26th week. The answer would change to appendicitis in that case.
A- Psoas
B- Rovsing
C- Obturator
D- Blumberg
Bad recall. Palpating the LLQ causes RLQ pain.
If C isn’t in the choices? Go with ileocecal valve.
A- Do the surgery and FU with US
B- Do the surgery and follow up with CTA
C-Do CTA before the surgery
A- Remove the appendix and close
B- Look for meckles diverticulum
C- Do open surgery and explore
D- Close without doing anything
Missing information. Was it laparoscopic or open? If you go for an appendectomy and during the procedure you discover a normal appendix go ahead and search for Meckel’s diverticulum. Afterwards, what we do next depends:
If open -> proceed with appendectomy If lap -> leave the appendix
Refer the patient to gastroenterology as it’s a case of IBD.
WBC high
US done showing appendicieal mass with NO collection What to do:
Small collection. Conservative care followed by an interval laparoscopic appendectomy.
Same approach we took with the prior patient.
Imaging: appendicitis, fecolith, appendicular abscess 10 x 15 cm reaching the flank. What is the management?
A- Open drainage
B- Percutaneous drainage
C- Open appendectomy with drainage
D- Laparoscopic appendectomy with drainage
Large collection this time. Drainage then interval laparoscopic appendectomy.
Old age? Colonoscopy.
Base of the appendix. Review the approach outlined at the start of this section.
 Hernia
Hernia
Small bowel obstruction is mainly mechanical, and hernias are the most common cause for SBO in a non-operated abdomen. Adhesions is the most common cause if prior surgery exists. Paralytic illeus is another cause for SBO occurring after surgery and features a silent sluggish bowel on examination with no mechanical blockage, so you’ll need to check for electrolytes first. Nitrous oxide is C/I in a SBO case.
Almost all adult hernia cases are repaired through hernioplasty. Open hernia repair is preferred over laparoscopic, except in the following cases:
– Bilateral hernia
– Recurrent hernia
– Obese
If the previous repair was open go for laparoscopic, and the opposite is true.
Para-umbilical hernia (PUH)
If below 2cm go with suturing. Larger? Mesh repair.
An asymptomatic or minimally symptomatic reducible inguinal hernia in the co-morbid elderly patient doesn’t need repair as the risk of strangulation is low. Same scenario but irreducible? Go for urgent repair. What if it was femoral hernia instead? Always needs repair regardless.
Post operative
Pus oozing? Open the wound to let it drain. If it reaches the mesh? Remove the mesh as well.
Swelling only? This is a collection of serous fluid called seroma, which simply needs regular wound dressing.
Complications
Incarcerated -> irreducible only.
Obstructed -> mainly presents with SBO symptoms and air fluid level.
Strangulated -> mainly ischemia and necrosis causing skin color changes. In addition to potential SBO sx, the skin overlying the hernia is erythematous and tender on examination.
Urgent surgical exploration is indicated in any of these cases.
Pediatrics
Umbilical hernia -> observe until 5 years old, then go for herniotomy.
Inguinal hernia in a child? Always go for herniotomy.
Minimal time before lifting heavy weights -> 6 months Ideal time before lifting heavy weights -> 1 year
obstruction. Which of the following is the most likely cause?
X ray air fluid level
What is the intial management?
A- Paracentesis
B- gastrografin enema
C- expl laparotomy
D- NGT , analgesic, bowel rest
Most likely to be Adhesions due to the intestinal obstruction + hx of surgery and air fluid levels. A rigid abdomen is an indication for laparotomy but the patient is vitally stable so I think it’s a bad recall. Either way, if it truly came like this I would still go with D since the patient is stable and the question asked for an initial management.
Adhesions again. The best way to diagnose intestinal obstruction in general is through a CT scan.
WBC 12.6 (high) Plain abdominal x-ray: multiple air-fluid levels CT scan: multiple dilated loops of small bowel with a transition point in the distal small bowel, with some adjacent fat stranding. Which of the following is the most appropriate next step in management?
They have already done CT here. Our patient is stable so the next step is to observe and keep NPO. No role for colonoscopy and no need to jump straight to laparoscopy.
A case of paralytic illeus. It is linked to electrolytes imbalance.
A – Urine osmolarity
B – Urine K
C – Stool K
D – ECG
Hypokalemia? Go for an ECG because of the effect it has on the heart.
Since it is such a common cause of SBO, we have to rule out inguinal hernia first with a simple physical exam.
Since the patient is not complaining of pain at the moment there is no urgent need to head to the OR just yet, so we might as well perform a CT scan and evaluate further. What if he was still in severe pain? Urgent surgery, not in 2 hours.
In cases of inguinal hernia affecting the elderly, the decision to go for repair depends on how the severity of symptoms. Since the patient is minimally symptomatic he should be treated conservatively since the risk of complications is low.
A- Open repair with mesh
B- Repeai hernia
C- do nothing
This is a similar case, but the hernia here is irreducible, so this patient needs surgery. We prefer an open repair over laparoscopic except in the following cases: bilateral, recurrent (open repair hx), and an obese patient. An irreducible hernia implies one of a few possible complications: incarcerated, strangulated, or obstructed. All three need surgery regardless.
The same could not be said for femoral hernias. They always need repair because of the high risk of complications.
Since it’s bilateral.
one side extending to hemiscrotum. what is the appropriate thing to now?
Recurrent hernia.
On x-ray there was multiple air fluid level in abdomen. What type of hernia?
Let us analyze this one by one in an ascending manner.
Incarcerated and irreducible are the same thing, meaning they’re both excluded. Their only feature is an irreducible hernia, which often presents with the other types anyway. That leaves us with strangulated and obstructed. Obstructed may be irreducible and it mainly presents with SBO symptoms and an air fluid level.
Strangulated hernia may present with all of the above in addition to a tender hernia on examination and ischemic skin color changes. In other words, red skin. The keyword in this question is tender hernia, so the answer is strangulated.
Simply open the wound to let it drain. What if the pus reached the mesh? The answer would change to C. Another recall mentions that the mesh is “exposed” meaning it reached it.
Umbilical hernia in children depends on the age. Below 5 years old? Observe. Once the patient turns 5 we go for herniotomy.
-Right inguinal herniolomy
-Open repair
-Mesh repair
-Wait till 6 Yo
Inguinal hernia in children needs herniotomy now.
The minimum time before lifting weights is 6 months, but ideally we should wait for 1 year. It depends on what the question is looking for.
Gastrointestinal
Upper GI
Boerhaave syndrome (esophageal perforation) is characterized by rupture of the esophagus due to forceful vomiting.
Esophageal cancer
The most common type worldwide is SCC, the most common risk factor overall is smoking, and the most significant risk factor overall is Barret’s esophagus.
– The strongest risk factors for SCC is achalasia (x10) followed by smoking (x9). The cancer is located in the proximal-mid esophagus.
– The strongest risk factor for adenocarcinoma is metaplasia due to Barrett’s (>x10), followed by GERD (x5-7). The cancer is located in the distal portion of the esophagus.
Upper GI bleeding approach
ABC -> endoscopic dx / mx -> surgical mx if warranted -> chronic management
Peptic ulcer is the most common cause of upper GI bleeding and it may only present with bleeding initially. Suspect it in cases with NSAID use. Urea breath is essential to confirm eradication of H. Pylori as clinical assessment alone isn’t enough. It’s treated medically unless uncontrolled.
Duodenal ulcers
A known case of PUD who failed medical treatment had an endoscopy showing multiple ulcers in the antrum? Go for a partial distal gastrectomy.
To diagnose gastric cancer if suspected, go for an endoscopy with biopsy. To stage gastric cancer, go for an endoscopic ultrasound. Surgery is the definitive treatment.
Low grade mucosa lymphoid tissue (MALT) -> simply eradicate H. Pylori with medical treatment.
If the patient has repeated episodes of vomiting then starts to bleeds, it goes with Mallory Weiss which needs upper endoscopy regardless of patient status to confirm it before discharging the patient.
Erosive esophagitis presents with a metallic taste and retrosternal chest pain.
Esophageal varices is suspected in patients with signs of portal hypertension/abnormal LFT.
Lower GI
Lower GI bleeding approach
ABC -> NGT aspiration (if massive) -> colonoscopy -> if normal colonoscopy, TC99 to look for angiodysplasia
Diverticular disease (a complication of diverticulosis) is the most common cause of lower GI bleeding.
Diverticulitis presents with LLQ pain. Typically, treatment is conservative with antibiotics, but drainage is indicated for unstable patients or a large size collection.
Elderly + recurrent painless bleeding and normal mucosa on colonoscopy -> Angiodysplasia. Diagnosed with TC99/Nuclear scan. If we had the same case but for a pediatric age group? Then it’s a case of Meckel’s diverticulum. Same investigation.
Anal fissure -> Pain with defecation, itchy, and a crack will be seen. Preventable condition. Treated with lateral internal sphincterotomy.
Anal abscess -> swelling or mass, fever, painful, high WBC. Prolapsed pile -> painless, vitally stable
Thrombosed pile/hematoma -> painful, vitally stable
Simple low lying fistula -> Pain and discharge. May rupture. Treated with fistulotomy. The most common location is medial posterior.
Hemorrhoids grades and treatment
Old age patient with hemorrhoids? Always go for a colonoscopy first.
Complex fistula approach
Known case of Crohn’s? Go with an MRI. Unknown case? Go with colonoscopy to confirm Crohn’s as a perianal fistula may be the first presentation that makes us suspect crohn’s. Surgery for toxic mega colon is curative in ulcerative colitis, but not in Crohn’s disease.
Complex fistulas are recurrent, multiple, and mainly present with discharge. The first step after performing an MRI is to administer IV Abx, then Infliximab for recurrent cases.
Be careful, the Crohn’s case may present with a simple tender swelling without discharge, which is a case of typical abscess -> I+D
vomiting. On examination there was decreased breath sound in the left lower chest What is the most
likely concern?
Boerhaave syndrome.
Patient after esophageal balloon dilation for esophageal varices started to complain of difficulty in breathing and voice change.
What is the complication?
A- Bleeding
B- Perforation
C- Aspiration
Perforation after dilatation can have a couple of different effects depending on where it happened. Upper part near the larynx leads to voice change, while perforation in the lower part of the esophagus leads to epigastric pain.
The best is heller myotomy, and the initial choice is pneumatic dilatation.
Old age and anemia goes with esophageal cancer. In another recall, the patient is younger and there is no mention of anemia. Instead, she has an elevated ESR. Therefore, in that recall the answer is achalasia. Make sure to review the esophageal cancer related questions on most common/significant as they like to play around with that. Also, in high grade dysplasia SCC we go for surgery. But if low grade, give the patient PPI and follow up after 6 months.
While preparing her for CT scan, she had fresh blood & coffee ground in her NGT tube bag. Her vitals & HgB levels are normal.
What is the most appropriate diagnostic test?
A- Colonoscopy
B- CT scan
C- Upper GI endoscopy
D- Abdomen US
As discussed in the upper GI approach, once we stabilize the patient and insert an NGT we should prep for an endoscopy.
days later he developed ground coffee vomitus. What is the diagnosis?
The keyword is mechanical ventilation which led to sores.
What is the diagnostic modality of choice?
A – Upper GI endoscopy
B – Abdominal CT
denied any history of vomiting, constipation, diarrhea, and or hematemesis. The pain is located in the epigastric area with a feeling of Nausea. Upon examination. There is tenderness and rigidity, what is the
diagnosis?
History of NSAID use is classic for PUD.
A- Erect chest X-ray
B- Abdominal X-ray
C- Abdominal CT
D- Abdominal US
Perforated PUD. Order an erect x-ray to look for air under the diaphragm.
history Labs show mild anemia, all labs are normal except elevated urea level in blood, what is the diagnosis?
Hematemesis alone goes with PUD, as it’s the most common cause of UGIB.
What is the most likely diagnosis?
Here, the patient had episodes of vomiting before hematemesis occurred.
Metallic taste.
A-Erosive gastrisis B-PUD
C-mallory weiss syndrome D-Esophageal varices
The keyword is dilated esophageal bleeding.
A case of uncontrolled PUD leading to posterior perforation. The bleeding site is the gastroduodenal artery which needs to be ligated.
Anterior duodenal perforation treated with an omentum patch.
B— reassure and ask to come if it recur again C— prepare for urgent EGD
D— Discharge
A case of Mallory Weiss which requires an upper endoscopy regardless in all suspected patients. The vomiting was severe enough to cause tears in the esophagus that led to the blood coming out so why would I reassure and discharge before doing any further workup?
First step in massive lower GI bleeding to rule out UGIB. If not massive, direct colonoscopy. After NGT, go for a colonoscopy to investigate.
They did both NGT and colonoscopy here. Since the colonoscopy results show nothing of note, the next step is TC99 to look for angiodysplasia.
A- juvenile polyp
B- Michele’s diverticulum
C- Intussusception
D- hirschsprung disease
Similar presentation to angiodysplasia with the only difference being the age group.
Angiodysplasia IBD
Diverticulosis
Uncomplicated diverticulitis treated conservatively. Small size, and no air fluid level indicating perforation.
Bp was normal temp was 37.6 Radiology image
Collection of fluid 9×10 cm with inflammation of the sigmoid How would you manage
A-Exploratory laparotomy
B-Sigmoidectomy and anastomosis C-Percutanous drainage
Here, it is complicated diverticulitis which is managed with percutaneous drainage.
A- anal fissure
B- hemorrhoids
C- juvenile poly
D- Intusseption
If failed, lateral internal sphincterotomy.
Let us exclude one by one.
Fistula -> Pain and discharge. May rupture.
Fissure -> pain during and after defecation, itchy, and a crack will be seen. Abscess -> mass, fever, painful, high WBC.
On the other hand, anal hematoma/thrombosed pile -> pain and swelling, but vitally stable just like our patient.
What about prolapsed pile? Similar, but painless.
An example from the management outlined above. Grade 2 (spontaneously reduced) and bleeding, so the definitive management here is C. If not bleeding? D.
A- strictureplasty
B- right hemicolectomy
C- coservitve management
D- segmental resection with ileostomy
D according to aldilaijain.
A- Colonoscopy
B- MRI
C- Fistulogram
D- US
Depends. Known case of Crohn’s? MRI. Unknown? Colonoscopy.
A tender swelling without discharge which is a typical case of abscess. But what if it had discharge? That would be a complex Crohn’s fistula.
A- Pelvic MRI
B- BroadIVAntiBiotic
C- Swabandculture
D- increse inflixmal dose
Normally, we would order an MRI then give abx, and infliximab for refractory cases. But our patient is passing pus and he is already taking both azathioprine and infliximab which are immunosuppressants, making it easier for our patient to become septic.
Colorectal
Colorectal screening
Average risk patient Annual FOBT
Sigmoidoscopy every 5 years Colonoscopy every 10 years
If positive family hx and a first degree relative was diagnosed before turning 60 years old -> colonoscopy every 5 years. Otherwise, it’s every 10 years.
In any old patient with GI bleeding or anemia, go for a colonoscopy. If the case is clear for colorectal then at first you must reach the diagnosis with a colonoscopy, then CT for staging, then you start treatment. If the patient is currently obstructed, surgery is indicated to relieve the obstruction before we do anything else. It’s a general rule in any cancer case.
Right colon cancer -> bleeding/anemia. We do a colonoscopy in an old age patient if suspected.
Left colon cancer -> obstruction. Relieve the obstruction with a sigmoidectomy then go for a colonoscopy. No obstruction? Skip to colonoscopy.
A case of dilated colon without a direct mechanical obstruction? Suspect Ogilvie syndrome and go for a decompressive rectal tube.
A case of absolute constipation, U shaped colon, empty rectum? Suspect sigmoid volvulus and proceed with an endoscopy for detorsion then go for colonoscopy and semi-elective surgery. If failed or unstable? Hartmann’s procedure.
Mesenteric ischemia
A case of small bowel infarction due to a blockage in the superior mesenteric artery. Suspect it in patients with ischemic heart disease (or other cardiac causes like A-Fib) + diffuse abdominal pain for several hours.
Diagnosed with CT-A.
A- no need for screening for her case
B- Start now and every 5 years
C- Start at 50 years with annual colonoscopy
D- Strat at 50 with annual Fecal occult blood
Colonoscopy every 10 years Sigmoidoscopy every 5 years Annual FOBT
A- Colonoscopy every 5 years
B- Colonoscopy every 10 years
C- CT Colonography every 10 years
D- Fecal immunochemical testing every 5 years
Again, every 10 years. His mother was diagnosed at 69, but what if they diagnosed her at 59? In that case, we would go for colonoscopy every 5 years.
A-3-6 month B-3years
C-5 years D-no need
Repeat colonoscopy in 3 years.
What is the best next step?
A – Colonoscopy
B – CT abdomen
C – MRI pelvis
D – Sigmoidectomy
A case of large obstruction, hence why we need to go for surgery first. If the patient is not currently obstructed? Colonoscopy.
A- Anal Cancer
B- Rectal Cancer
C- condyloma accuminatae
The keyword is cauliflower like mass.
An example of right sided cancer with anemia.
Anemia, and red streaks of blood in the stool due to the location of the cancer.
110/70 mmHg 96 / min 18 / min 36.6 ° C CT scan chest: No evidence of metastasis. Which of the following is the most appropriate treatment?
A- Diversion colostomy
B- Low anterior resection
C- Concurrent chemoradiation
D- Abdominoperineal resection
In rectal adenocarcinoma, neo-adjuvent chemoradiation is a must regardless of the surgical procedure.
A/ Occult fecal blood
B/ Endoscopy & colonoscopy
Old age + anemia = suspect right sided cancer.
Abdominal Xray: dilated colon lumen 10cm CT: No obstruction
Best management?
a-Decompression colonoscopy with rectal tube. b-emergency colectomy.
c-Lt side colostomy.
d-lower barium enema.
Dilated colon without a mechanical cause. A case of ogilvie syndrome.
-Rectosigmoid cancer
-Sigmoid volvulus
-obstruction
-closed loop
The shape they are describing is U, in addition to a coffee bean sign on xray.
B, CT-A is more correct.
Most likely a case of mesenteric ischemia although ischemic colitis is another DDx and we use CT for it.
Another recall:
dx?
Hepatobiliary
US is always the first step, even if the patient is obese.
Ascending cholangitis
Charcot triad needs to be present in order to complete the diagnosis: 1) Fever 2) RUQ pain 3) Jaundice. Treatment is drainage by an ERCP.
Biliary Pancreatitis
It can cause epigastric or RUQ pain. Dilated CBD is key. It doesn’t complete the Charcot triad, and it doesn’t have features suggesting cholecystitis.
Initially, in pancreatitis cases we order serum amylase/lipase (the latter is preferred) and an US. In a severe or late presentation, go with CT abdomen and look for necrotizing pancreatitis.
Cholecystitis
History of biliary colic after fatty meal, fever, and RUQ pain. No jaundice.
No CBD dilatation. Positive Murphy’s sign.
The golden period for cholecystectomy is in the first 72h, but if the patient is past it manage conservatively then schedule for elective lap chole in 6 weeks.
A symptomatic patient had an US showing sludge? It’s essentially a small stone so go for lap chole.
Let’s suppose we had an incidental finding of gall stones in an asymptomatic and stable patient, next? Reassure without further follow up as this is very common.
ERCP for a dilated CBD is always done before lap chole, but both are done in the same admission.
Hx of MI patient with a stent? Elective lap chole in 6 weeks.
Lap chole complications
Stable -> US -> drainage -> ERCP definitive Unstable (or peritonitis) -> laparotomy
Biliary pain in a pregnant patient? Start conservatively if possible, and go for lap chole if there’s recurrent attacks, uncontrolled symptoms, or no weight gain. The safest time for lap chole is in the second trimester.
Klatskin tumor -> shrunken gall bladder, dilated intrahepatic ducts. Pancreatic cancer -> enlarged gall bladder, dilated intrahepatic ducts.
Ampullary cancer -> dilated extrahepatic and intrahepatic ducts.
Gallstone illeus presents with abdominal pain and hx of gallstones years ago. Classic triad of:
Hemochromatosis
Ferritin >300 Transferrin saturation (TSAT) >45%
Elevated serum iron Decreased TIBC
Alcoholic hepatitis Very high AST and ALT AST/ALT ratio 2:1
Case of diabetic pt with no lab values? Go with NAFLD as it’s very common.
Primary biliary cirrhosis -> antimitochondrial antibodies (AMA)
Autoimmune hepatitis -> antinuclear antibodies (ANA), and anti-smooth muscle antibodies (ASMA). High AST ALT.
Primary scelrosing cholangitis -> associated with UC (diagnosed by colonoscopy if suspected). Go for MRCP to confirm.
HCC
Positive antibody but negative RNA?
– If no symptoms, no recent exposure, no abnormal labs, then no need for follow up.
– If there is a possible recent exposure, repeat RNA in 6 months.
– If the patient is currently symptomatic repeat RNA now.
Screen for HCC with US, then confirm the diagnosis with triphasic CT. Regular follow up every 6 months with an US if cirrhosis is present.
Treatment
5cm+ or multiple nodules, go with TACE. Otherwise, go with surgical excision.
C/I for a liver transplant:
Liver mass
The most important step is to avoid contact sports in hemangioma. Female patient taking OCP? It’s an adenoma so stop OCP. If neither are present in the choices, then go with decrease carbohydrates and fatty meals.
right upper quadrant tenderness, no history of medication or disease, what is initial step?
Ultrasound: CBD of 1.4 cm with dilatation of intrahepatic ducts. Which of the following is the most likely diagnosis?
Charcot triad. Cholangitis is treated with an ERCP.
Exam :mild epigastric tenderness previous multiple hospitalization Labs : amylase normal
Bp. 110/69 Hr 110
Dx?
A- Acute pancreatitis
B- chronic pancreatitis
C- esophgial varisis
D- pancratic psodocyst
Heavy alcoholic and multiple hospitalizations.
No Charcot triad, and the findings are not relevant for cholecystitis.
Classic case of cholecystitis. The patient presented in the first 72h so go for lap chole. But if past it? Treat conservatively then schedule for elective lap chole in 6 weeks.
Sludge is a small stone. Treat it just like you would with a typical cholecystitis.
U/S shows small gall bladder stones & 5 mm polyp, what is the management?
Lap chole.
Observation
Radical cholecystectomy Repeat US after 3 months
If any of the following are present refer for surgery:
Otherwise? No need for follow up.
ERCP then lap chole in the same admission.
perforated?
A- do it in this admission
B- delay it 6 weeks
C- delay it 6 months
D – no need to do it anymore
Antibiotic therapy was started. What is the next step?
We did the US in the prior question, so time for drainage.
Vitally unstable or has peritonitis? Laparotomy. Definitive? ERCP after US and percutaneous drainage.
Which of the following is the most appropriate management?
A- Acute Cholecystitis
B-Gall Bladder Stone C-CBD Stone
D- klatskin tumor
Labs: cholestatic picture
(They did not mention if the gallbladder is palpable or shrunk 🙂 )
and fatigue There was air in biliary system, what is the diagnosis?
A- Gastrograffin test
B- Barium swallow
C- Abdominal CT
D- US
Go for CT in gallstone illeus.
A-hemochromatosis B-alcoholic hepatitis C-cholangitis
AST/ALT ratio 2:1? Alcoholic hepatitis. If the labs simply showed high ferritin the answer would be A. Now, what if we had no lab values at all in the question in a case of a diabetic patient? Go for NAFLD.
what is the diagnosis?
First, we have to do an US. Afterwards, for further workup it depends: Autoimmune hepatitis -> ANA, ASMA
Primary biliary cholangitis -> AMA. Primary sclerosing cholangitis -> MRCP
MRCP: multiple foci of stricture and dilatation. What is best initial next step?
This is a very similar case. We should look for ulcerative colitis due to the association between the two.
US guided cholecystostomy tube Urgent open cholecystectomy
This ICU patient is unable to tolerate lap chole, so go for cholecystostomy tube.
A case of metastatic liver cancer. Colorectal cancer is the most common cancer metastasizing to the liver.
A-Hepatocellular carcinoma B-pancreatic cancer
A – Chemotherapy
B – Radiotherapy
C – Transcatheter arterial chemoembolization (TACE)
D – Surgical resection
Due to the presence of cirrhosis.
What to do ?
A- Liver biopsy
B- Liver ultrasound
C- Repeat HCV RNA after 6m
D- No need for further intervention
If symptomatic, repeat RNA now. If the patient had recent exposure, repeat RNA in 6 months.
Abdominal US Triphasic CT
Screening? Ultrasound. Confirmatory? Triphasic CT. Could be a bad recall, but since it mentioned screening specifically the best way is with an US. Another recall: What is a risk factor for HCC? Hepatitis B.
LDH, US done and showed unremarkable findings, what is the diagnosis?
Pancreatic pseudocyst
We suspect pseudocyst in cases with a history of pancreatitis weeks ago followed by epigastric pain that makes the patient return. Regardless, the investigation of choice is always CT scan even if asked for an initial investigation. US is wrong.
We typically observe these cases, but if one of the following is present go for endoscopic drainage.
6+ weeks history or 6cm+ collection.
Pseudocyst -> homogenous fluid. Endoscopic drainage. Most common presentation.
Walled off necrosis -> heterogenous fluid. Percutanous drainage as it’s infected.
Pancreatic abscess -> presents with fever. Percutanous drainage.
If the question doesn’t specify what kind of collection and fluid? Go with endoscopic (internal) drainage because that’s the most common scenario.
The only exception to the 6 weeks / 6cm size rule is in infected cases. Go for a percutaneous (external) drainage regardless of how long it’s been or how big the collection is because the patient is currently infected and needs intervention.
Liver abscess
Hydatid liver disease Organism: Echinococcus Initial: Albendazole
Definitive: Surgical deroofing (especially if daughter cysts are present).
Amebic liver disease
Organism: E. Histolytica. History of traveling to India/Mexico or another endemic area is an important keyword. Solitary hypodense cystic lesion. Amebiasis also causes dysentery (bloody diarrhea) if it infects the intestines, so that’s another keyword. Patient may be febrile for a long duration. Treated with Metronidazole.
Pyogenic liver disease
Most common liver abscess in developed countries. Features of thick walled hypodense fluid cavity on CT. Occurs secondary to infection, most commonly cholangitis. May have elevated liver enzymes. Initiate management with a broad spectrum antibiotic in all patients. Most patient may require percutaneous drainage as well.
Temp. 37.9 (I think but it was elevated) wbc high, bilirubin high US: cystic lesion without septates CT : homogenous (not sure) and “THICK WALL with
Peripheral enhancement
– What’s most appropriate
Case of pyogenic liver abscess, which is the most common cause of liver abscess by far in developed countries. The most appropriate management is drainage. As for the initial step, go with Ceftriaxone since we have to start it in all patients in addition to drainage.
As mentioned previously pyogenic abscess is the most common one, but since the patient came from India and has been febrile for 3 weeks we will go with amebic abscess.
Mexico is another endemic area for amebic abscess. What if we removed it from the question? The answer would change to A.
What is the most likely diagnosis?
Heterogenous fluid, making it a case of walled off necrosis. If homogenous fluid? Pseudocyst. If febrile? Abscess. What if none of it was mentioned to begin with? Pseudocyst since it’s the most common presentation.
(Didn’t specify homogenous OR heterogenous)
No fever, and no mention of a heterogenous collection.
4 weeks and 4cm, so keep observing for now. Afterwards, go for internal drainage.
A- Percutaneous drainage
B- Endoscopic drainage
C- Surgical drainage
No additional details that would change the answer (fever/heterogenous), so go for endoscopic drainage.
-laproscopy drainage
-percutaneous drainage
-excision of the cyst
-I dont remember maybe it was observe
Bad recall. There are two possible explanations:
Post-op infection
SSI approach
Open wound -> CT to assess for possible deep infection -> percutaneous drainage
Intra abdominal collection
Abx if small size, percutaneous drainage if 4*4 or bigger, laparoscopy if multiple collections, and laparotomy if the patient is unstable.
“Open drainage” isn’t the same as open the wound. It refers to percutaneous drainage which is done after CT, so be careful. The proper way to drain percutaneously/externally is through CT-guided drainage.
Open the wound = remove stitches/clips = I&D.
A case of abscess? Simply go for an incision & drainage.
post surgery with wound site redness & tenderness with purulent discharge.. most appropriate?
A-Laproscopic drainage B-Percutaneous drainage
C-Open drainage
D-Open drainage with fistula resection.
has seroma which drains freely from the opening of the wound, no erythema no pain no fever, what is the
appropriate management?
A case of a serous fluid collection called seroma.
ABC
A
All are indications to intubate.
In addition, we use an oxygen mask as pre-oxygenation for a conscious alert patient, but the best way is orotracheal intubation if the patient is unconscious or moaning. Let’s suppose the same patient had a face fracture (mandible), in that case go for a cricothyrotomy.
B
Typically in cases such as tension pneumothorax which is treated by needle decompression. Never choose needle decompression before intubation as it’s wrong in the SMLE despite what UTD says. Follow the sequence.
C
IV fluid and circulation control, then proceed with imaging if no disabilities exist.
Always follow ATLS in every case before choosing anything else.
Severe vomiting -> hypochloremic hypokalemic metabolic alkalosis (loss of Cl and K). Treated with normal saline.
Severe diarrhea -> metabolic acidosis (loss of HCO3 and K). Treated with ringer lactate.
Both hypokalemia and hyperkalemia affect the heart rhythm. Hypokalemia (Flat T wave) is treated with oral potassium.
Hyperkalemia (Peaked T wave) is treated with calcium gluconate, and the second line is SABA/Insulin. Dialysis for refractory cases.
Severe hyponatremia (NA below 120) -> neurological symptoms.
Treated with hypertonic saline.
Feeding
If the patient doesn’t have an adequate oral intake, we need to provide nutrition in an inpatient setting. First, check the GI function, if it’s not functioning properly start with parenteral nutrition (IV access).
Otherwise, enteral feeding is indicated. An acute case below 1 month?
Start with NGT. Risk of aspiration? Go with NJT. Both are initial measures if the question asked for such.
A chronic case more than 1 month?
Initiate resuscitation with gastrostomy. Risk of aspiration? Go with jejunostomy. Both are considered the most appropriate management/ best in a chronic case.
Wound closure
As explained earlier. Also, in the full recall they asked for next.
This patient has problems in both A and C. Prioritize the airway and go for an endotracheal intubation since the patient is unconscious.
Because of the face fracture.
How will you secure the airway?
A – Tracheostomy tube
B – Cricothyroidotomy
C – Orotracheal tube
D – Nasopharyngeal airway
Similar question but in a pediatric age group. A according to Thawaba.
A Intubation and 100% oxygen
B. Rapid infusion of crystalloid
C. Needle decompression D IV 0.2 mg adrenaline
Always go with ABC. Intubate then go for needle decompression.
80/60
Pules 133
RR 25
O2 88%
How to manage him?
Why rush to laparotomy? The patient is desaturated.
A- inhalation injury
B- carbon monoxide toxicit
A- elective intubation
B- ICU observation
C- advice patient to take analgesia
Bp : 110/80
Temperature : 37.2
HR : 88
RR : 19
what’s the type of fluid replacement will give?
A – normal saline
B – half NS
C – hypertonic saline
Indication of hyperkalemia treatment:
A initially, then B, then C for refractory cases.
is your priority?
We need to maintain the circulation, the rest are not as important.
is the next step?
Primary survey. A simple and fast physical exam should always be the first step.
A- Direct pressure on the wound
B- pressure above the wound on femoral artery
C- apply tourniquet
Different scenario. The first one is asking about the most appropriate method to provide feeding for the patient (best), and the second question is asking us the most appropriate way how to initiate feeding. NJT would be better than NGT since the patient is at risk for aspiration.
Primary suturing/closure as it’s within the 24 hour window.
Primary repair to injured structures as it reached the tendons and nerves.
management?
Exposed necrotic skin, so go with secondary closure.
VAC. No signs of infection.
Lung nodule approach
First, check if a previous chest X-ray exists.
If the lung nodule hasn’t changed in 2-3 years, then no need for further follow up.
More than 2cm -> surgery Between 0.8mm and 2cm -> PET or Biopsy
More than 0.4mm but less than 0.8mm -> CT scan follow up 0.4mm and below, no need for follow up
Always the first step.
No change in the size for 2 years.
0.5mm – 0.7mm = CT
If 0.4mm or below? No need for follow up.
If you see both PET and Biopsy in the choices, go with PET. Patient stopped smoking 20 years ago? Irrelevant detail which does not change anything as the nodule is still 1cm.
Because the nodule is rapidly growing in such a short time, it would be best to refer the case.
Obesity
Bariatric surgery is the best way to reduce weight.
Indicated in a BMI of 40+ or 35+ in a co-morbid patient. You may have to calculate it yourself. The next best way after surgery is lifestyle, then Orlistat.
To choose the type of procedure, we perform an endoscopy.
Hx of roux-en-Y bypass -> internal hernia Hx of sleeve gastrectomy -> adhesions
Patient post bypass surgery? Go with CT even if unstable.
Patient post sleeve surgery? Go with endoscopy.
Jejunum -> folic acid absorption Terminal ileum -> vitamin B12 absorption
If either of the two are tampered with in a bypass surgery? It eventually causes megaloblastic anemia, so those patients need parenteral replacement.
The very best is surgery, followed by lifestyle modification. The third best is a medication called Orlistat. Remember, we can only offer bariatric surgery in patients with a BMI of over 40, or over 35 if co-morbidities exist.
A, even if the blood pressure is 90/60 in another recall. If the patient presented after sleeve, go with endoscopy.
What is the likely diagnosis?
A – Incisional hernia
B – Internal hernia
C – Intussusception
D – Adhesion
Hx of sleeve. If hx of roux-en Y, choose internal hernia.
A- gastric leakage
B- sepsis
C- decreased oral hydration
D- inadequate analgesia
A according to Thawaba.
Acute Limb Ischemia
ALI approach
Heparin – US – CT-A (skip if paralyzed limb/class III) – Angiography
PAD approach
Heparin (only if acute on chronic, skip otherwise) – ABI – US – Angiography for revacularization as the definitive management in CLI.
A supervised exercise program to increase the walking distance, and smoking cessation is a must in PAD. Aspirin to prevent cardiovascular events.
Absent pulse is the first sign in all classes of ALI. Class 1 -> Moderate pain
Class 2 -> Severe pain, moderate sensory loss and
paraesthesia
Class 3 -> No pain, paralyzed limb
Treatment
Choose amputation if it’s an acute on chronic case or if irreversible paralyzed limb (class III), embolectomy if A-Fib or other cardiac cause. Catheter thrombolysis is used in arterial thrombosis and is also preferred over embolectomy as a first line treatment in ALI (IV tPa is wrong in limb ischemia, you only choose it in stroke/MI/PE).
Foot ulcers
If the pulse is absent, that indicates an arterial issue as discussed in the ALI section so go with arterial US next. If the pulse is intact and there is a dark skin discoloration, go with venous US. The most common risk factor for a venous ulcer is venous hypertension, followed by age.
AAA approach
Symptomatic and stable – CT-A Asymptomatic and stable – US (screening) Unstable and unknown case – US
Unstable and known case of AAA – immediate laparotomy
Cardiac = embolus. Acute arterial embolus presents more acutely than thrombosis.
Cardiac related, so this is caused by an embolus. The best treatment is embolectomy.
US after Heparinization.
Right leg: palpable femoral and poplitteal. dista veins are not palpable.
-What is the appropriate investigation?
Most appropriate investigation (not next step) -> CT-A
Catheter thrombolysis is preferred unless they give history of a cardiac cause.
What is the most appropriate management ?
As explained earlier, cardiac cause? Embolectomy.
A- amputation
B- thrombolysis
C- embelctomy
A case of acute on chronic. Chronic history of PAD followed by an acute episode of ALI.
A- Varicose vein
B- Arterial causes
C- infection
D- Diabetic neuropathy
Clear case of peripheral artery disease.
Start with an ABI then go for an US.
A- CTA
B- vascular ultrasound
C- conventional Angio
D- MRA
US next, angiography best.
A to improve his walking distance specifically, but smoking cessation is superior overall.
Which one of the following indicates acute limb ischemia:
A-intermittent claudication
B-rest pain
C-scar for iliofemoral bypass in left leg D-swelling
Rest pain goes with ALI. Intermittent claudication goes with PAD/chronic limb.
A- Diabetic
B- Venous hypertension
C- Atherosclerosis
D- Buerger’s disease.
and viable ulcer bed, best next step is?
US initially. In this case, venous US because of the dark discoloration and a viable ulcer bed.
If dietary modification isn’t in the choices, go with debridement.
As a general rule, whenever you encounter a question in the Qbank that goes like “case of X” it means they were giving you the symptoms, not the diagnosis. “Known case of” is a different story.
PE approach
Features of massive PE:
PE Treatment
LMWH or fondaparinux are preferred over UFH Choose tPa/thrombectomy if unstable pt or massive/saddle PE
Rivaroxaban if it’s about chronic management
DVT Treatment
LMWH (pregnancy, cancer case) 40mg is prophylactic
40mg BID is therapeutic
UFH (renal impairment) 5k IU BID is prophylactic 10k IU is therapeutic
In severe DVT cases that mimic ALI by having ischemic changes, the answer changes to tPa, or IVC filter if tPa is C/I (for example stroke, or the patient is post-op in the recovery room).
A- Ct
B- D dimer
C- V/Q
D- Us for lower limbs
Compressed US initially, but if it fails go with V/Q scan as the definitive choice for a pregnant woman.
What is the confirmatory test?
A..spiral ct B..echo C..ecg D..dimer
In the exam, the ECG was probably showing sinus tachycardia. Go for D if asked for an initial test.
A – PE
B – cerebral infraction
C – brain hemorrhage
D – arrhythmia
History of a bedridden patient eventually leading to massive PE with ECG changes and CNS symptoms.
A- warfarin
B- enoxaprin
C- thrombolectomy
saddle = massive. Go for thrombolysis/thromboectomy, whichever is in the choices.
Heparin infusion TpA
most appropriate management
A- Aspirin
B- Foundaparinux
C- IV heparin (no enoxaparin)
D- Revaorxaban
LMWH would be preferred, so with these choices go for B. According to UTD, Rivaroxaban is more suitable to be used as an indefinite anticoagulant management but for this case we need an acute treatment. UFH is less useful in PE.
To prevent DVT, choose a prophylactic dose as outlined earlier.
A- Aspirin 61 mg
B- Enoxaparin 40 mg SC
C- Fondaparinux 20 mg
D- Hepatin 10,000 U IV
Since the patient already has DVT, we need a therapeutic dose.
The keyword is patient in the recovery room. This is a case of PCD (severe DVT with absent pulse) which is typically managed by thrombolysis but it’s contraindicated due to the recent surgery within 24 hours.
A somewhat similar case of post-op DVT becoming severe enough to cause limb ischemia, so the first line treatment should be thrombolysis. In another recall thrombolysis isn’t available, so in that case go for heparin.
Orthopedics
Supracondylar fracture approach
Urgent reduction, then K-wire if pink and warm, surgical exploration if pale and cold. (If you have to choose between the last two and the question is vague, go with K-wire).
Lower limb fractures
Adults -> Close reduction with intramedullary nail
Children
Less than 6 months -> Pavlik harness 6 months to 5 years -> Hip spica More than 5 years -> IM nail
Open fracture approach
IV antibiotics -> close reduction -> debridement -> definitive with IM nail or external fixation if extensive soft tissue damage.
Compartment syndrome
Pain (1st alarming sign), Paraesthesia (2nd alarming sign), Pallor Pulseless, Paralysis. Urgent fasciotomy.
Pelvic fracture
Stabilize the pt with ringer lactate and a pelvic binder, then head to the OR.
Fat embolism mimics Pulmonary embolism, but the main difference is that FE has CNS symptoms and petechial rash.
Most common shoulder dislocation is anterior (Abduction and external rotation). However, posterior dislocation occurs in epileptic patients.
Most common hip dislocation is posterior (abduction and internal rotation).
A- oral antibiotic
B- open fixation
C- surgical debridement
D- external fixation
IV antibiotics, then debridement.
What is the definitive management?
Typically, open reduction (not close) and fixation with IMN which is also referred to as ORIF is the definitive treatment, but in this question we need an external fixation because of extensive soft tissue damage. C would be initial.
Initially, we go with close reduction then the next step depends on the temperature and color of the skin. But what if the question was vague? Choose K-wire.
What is your management?
What is your management?
What is the definitive management?
What is your working diagnosis?
The patient was given ringer lactate already, so the next step is pelvic binder, and the definitive is operative fixation.
Another recall:
After operation he became confused and developed dyspnoea, petechiae and tachycardia. What is the most likely diagnosis?
The keywords to differentiate between PE and FE: CNS symptoms and petechial rash.
Urology
Testicular torsion -> less than 12h with horizontal high riding testis, and absent cremastric reflex. Severely tender testis. Urgent surgical exploration.
Appendicular torsion -> typically less than 1 day with vertical/longitudinal, blue dots sign, and upper pole tenderness. Decreased vascularity on US.
Epididymitis -> typically more than 1 day, edematous, with an increase in vascularity on US.
Incarcerated inguinal hernia -> unilateral swelling which extends to the inguinal region, and the testis cannot be palpated.
Hydrocele -> positive transillumination test and no pain.
Trauma
Intraperitonal injury -> surgical exploration Extraperitoneal injury -> catheter repair then reassess 2 weeks later
Urethral injury -> suprapubic catheter, if not available choose retrograde urethrogram to diagnose. Foley’s is C/I in urethral injuries.
The most significant risk factor for malignancy in a patient with BPH is age.
Undescended testis
Palpable under general anesthesia? Go for orchidopexy.
Still not palpable? Go for diagnostic laparoscopy.
Next step
Gross hematuria -> Urine cytology Microscopic hematuria -> Repeat urinalysis
Elderly painless hematuria -> Cystoscopy Elderly painful micturition -> Foley’s catheter
Small stones pass spontaneously and need no intervention.
A-Testicular torsion
B-Appendicular torsion C-Cry..orchitis
D- Hydrocele
A- testicular torsion
B- Epidydomorchitis
C- Incarcerated inguinal hernia
D- Testicular appendicular torsion
hydrocele Cyctocyle
cystoscopy folly catheter
retrograde urthrogram fluoroscopic cystogram
the most appropriate to do?
canal and small in size and easily moved to scrotum, the left is normal, what is the cause?
A- Cystoscopy
B- CT abdomen
C- Iv pyelogram
D- Us
A- Abx for uti
B- Foley catheter
C- Cysoscopy and turp
repeat urinalysis Urine cytology Renal Biopsy Cystoscopy
A-Ask for serum creatinine
B- Do Serum albumin
C-repeat urine analysis in few days
D-Send her for biopsy
Exercise induced microscopic hematuria.
Below are some repeated questions.
Grade A vs Grade B.
peri operative management?
diagnosis?
A- Incentive spirometry
B-Chest tube
C-Needle decompression
Case of atelectasis.
pain. What is the diagnosis?
Physiotherapy next, spinal leminectomy best.
conscious and alert. Examination showed 5 cm x 11 cm wound at her back with burned clothes and powder of chemicals on her clothes and skin
Which of the following is most appropriate next step after removing her clothes?
A- normalization of heart rate
B- normalization of blood pressure
C- Urine out of 0.6ml/kg/h
D- Central venous pressure 12
He is afebrile. What
is the most likely diagnosis?
In the full recall the patient didn’t have high WBC.
A- iv mannitol
B- elevate head of bed
C- hyperventilate
D- urgent craniotomy
A- Mastoid
B- Maxillary
C- Basal skull
A-Nystagmus
B-Ventricular tachycardia C-Drowsiness
abdominal pain. Imaging of the spleen showed a 7 mm hematoma and 4 cm tear (grade 3).
Your management is?
Only go with splenectomy if the patient is unstable
presented 4 months later with depressed mood and fatigability. Both parathyroid hormone and calcium
were high, what is the most common cause?
Less than 6 months -> missed adenoma
More than 6 months -> parathyroid hyperplasia
A Sclerotherapy
B Endovenous laser
C Thermal ablation
increase the safety of patients undergoing surgery. The Checklist consists of three phases of surgical
procedure: